Medical Device Applications Guide
Comprehensive guide to metallographic analysis for medical device applications, covering biocompatible material preparation, surface finish requirements, implant material characterization, and regulatory compliance considerations.
Table of Contents
Introduction to Medical Device Metallography
Metallography in medical device applications presents unique challenges and requirements that differ significantly from industrial metallography. Medical devices, particularly implants, must meet stringent biocompatibility, surface finish, and regulatory requirements that directly impact patient safety and device performance.
This guide addresses the specialized metallographic techniques required for medical device analysis, with emphasis on biocompatible materials (primarily titanium, stainless steel, and cobalt-chromium alloys), surface finish characterization, implant material evaluation, and compliance with medical device regulations.
Critical Considerations: Medical device metallography requires strict contamination control, detailed documentation for regulatory compliance, specialized techniques for surface analysis, and understanding of biocompatibility requirements. Patient safety depends on accurate and thorough analysis.
Biocompatible Material Preparation
Biocompatible materials used in medical devices require careful preparation to avoid contamination, preserve surface characteristics, and maintain material integrity. The most common biocompatible metals are titanium and its alloys, stainless steel (316L), and cobalt-chromium alloys.
Titanium and Titanium Alloys
Titanium is widely used in medical implants due to its excellent biocompatibility, corrosion resistance, and strength-to-weight ratio. Common alloys include commercially pure titanium (CP Ti) and Ti-6Al-4V.
Titanium alloy microstructure, 400X magnification (DIC). Proper preparation reveals alpha and beta phases critical for implant performance.
Preparation Considerations
- Contamination control: Titanium is highly reactive. Use clean, dedicated equipment and avoid cross-contamination with other materials
- Sectioning: Use slow cutting speeds and appropriate coolants to minimize heat generation and prevent surface oxidation
- Mounting: Use compression mounting with appropriate pressure to avoid deformation. Consider castable mounting for porous or delicate structures
- Grinding: Use progressive grinding with SiC papers. Titanium work-hardens easily, so use light pressure and frequent cleaning
- Polishing: Use diamond polishing compounds (3 μm, 1 μm, 0.25 μm). Final polish with colloidal silica or alumina suspension
Etching for Titanium
Common etchants for titanium alloys:
- Kroll's reagent: 2-3 mL HF, 5-6 mL HNO3, 100 mL H2O. Reveals alpha and beta phases in Ti-6Al-4V
- Modified Kroll's: For better contrast, adjust HF concentration
- Weck's reagent: For color contrast, especially useful for distinguishing phases
- Anodizing: Use anodizing techniques for grain structure analysis
Safety note: HF is extremely hazardous. Use proper PPE, fume hoods, and follow all safety protocols. Consider alternatives when possible.
Microstructure Evaluation
- Assess alpha and beta phase distribution in Ti-6Al-4V
- Measure grain size per ASTM E112
- Check for alpha case (surface contamination layer) that can affect biocompatibility
- Evaluate microstructure uniformity
- Document any undesirable phases or structures
Stainless Steel (316L)
316L stainless steel is commonly used in medical devices due to its corrosion resistance and biocompatibility. The "L" designation indicates low carbon content, which minimizes sensitization.
Stainless steel microstructure, Kalling's No. 2 etchant, 400X magnification. Proper austenitic structure is essential for medical device biocompatibility.
Preparation Considerations
- Standard metallographic preparation techniques apply
- Use progressive grinding with SiC papers
- Polish with diamond compounds followed by colloidal silica
- Maintain cleanliness to avoid contamination
Etching for 316L
- Electrolytic etching: 10% oxalic acid, 6V DC, 5-10 seconds. Reveals grain boundaries and sigma phase
- Glyceregia: 15 mL HCl, 10 mL glycerol, 5 mL HNO3. General purpose etchant
- Aqua regia: For revealing carbides and sigma phase
Microstructure Evaluation
- Verify austenitic structure (no ferrite or martensite)
- Check for sigma phase formation (brittle intermetallic)
- Assess grain size
- Check for sensitization (grain boundary carbides) that can lead to intergranular corrosion
- Document inclusion content per ASTM E45
Cobalt-Chromium Alloys
Cobalt-chromium alloys (e.g., CoCrMo) are used in joint replacements and other high-wear applications due to their excellent wear resistance and biocompatibility.
Preparation Considerations
- Cobalt-chromium alloys are very hard. Use appropriate cutting and grinding techniques
- Use diamond polishing compounds throughout
- May require longer polishing times due to hardness
- Use light pressure to avoid relief between phases
Etching for Cobalt-Chromium
- Murakami's reagent: 10g K3Fe(CN)6, 10g KOH, 100 mL H2O. Colors carbides
- Glyceregia: For general microstructure
- Electrolytic etching: Various electrolytes can be used
Microstructure Evaluation
- Assess carbide distribution and morphology
- Evaluate grain structure
- Check for proper heat treatment structure
- Document any undesirable phases
Contamination Control
Contamination control is critical in medical device metallography:
- Use dedicated equipment for medical device samples when possible
- Thoroughly clean equipment between samples
- Use clean, filtered polishing media
- Avoid cross-contamination between different materials
- Document cleaning procedures
- Consider using disposable consumables for critical samples
Surface Finish Requirements
Surface finish is critical in medical devices, particularly implants, as it affects osseointegration, wear resistance, and biocompatibility. Metallographic analysis must accurately characterize surface finish without introducing artifacts.
Surface Roughness Measurement
Surface roughness affects implant performance:
- Ra (arithmetic average): Most common parameter, typically 0.1-2.0 μm for implants
- Rz (average maximum height): Peak-to-valley measurement
- Rt (total height): Maximum peak-to-valley distance
Use profilometry or interferometry for quantitative measurements. Metallography provides qualitative assessment and cross-sectional analysis.
Cross-Sectional Surface Analysis
Prepare cross-sections perpendicular to the surface to evaluate:
Surface Topography
- Surface roughness profile
- Surface texture characteristics
- Coating or surface treatment thickness
- Surface modification depth
Surface Integrity
- Absence of cracks or defects
- Proper surface treatment application
- Surface contamination assessment
- Oxide layer evaluation (for titanium)
Surface Treatment Evaluation
Many medical devices undergo surface treatments to enhance performance:
Anodizing (Titanium)
- Measure anodized layer thickness
- Assess layer uniformity
- Check for proper anodizing coverage
- Evaluate layer adhesion
Plasma Spray Coatings
- Measure coating thickness
- Assess coating porosity
- Evaluate coating-substrate interface
- Check for delamination or cracks
- Assess coating microstructure
Acid Etching
- Evaluate surface texture created by acid etching
- Assess etching depth and uniformity
- Check for over-etching or under-etching
- Document surface morphology
Sandblasting/Grit Blasting
- Assess surface roughness
- Check for embedded particles
- Evaluate surface damage
- Document surface texture
Preparation for Surface Analysis
Special considerations for surface finish analysis:
- Section perpendicular to the surface
- Use appropriate mounting to preserve edges
- Avoid rounding of edges during grinding and polishing
- Use edge retention techniques (e.g., nickel plating, specialized mounting)
- Maintain flat surfaces for accurate measurements
- Consider using scanning electron microscopy (SEM) for detailed surface analysis
Surface Contamination Assessment
Check for surface contamination that can affect biocompatibility:
- Metallic contamination from processing
- Organic contamination
- Oxide layers (desired or undesired)
- Embedded particles from surface treatment
- Residual processing materials
Use appropriate analytical techniques (EDS, XPS) in conjunction with metallography to identify contamination types.
Implant Material Characterization
Comprehensive characterization of implant materials ensures they meet specifications and perform as intended in the body. This includes microstructure, mechanical properties, and biocompatibility-related features.
Microstructure Characterization
Detailed microstructure analysis for implants includes:
Grain Structure
- Grain size measurement per ASTM E112
- Grain shape and distribution
- Grain boundary characteristics
- Texture assessment (for wrought materials)
Phase Analysis
- Phase identification and distribution
- Phase volume fraction measurement
- Phase morphology assessment
- Presence of undesirable phases
Precipitate and Inclusion Analysis
- Precipitate size and distribution
- Inclusion content and type
- Intermetallic phase assessment
- Documentation per applicable standards
Porous Structures
Many implants use porous structures to promote bone ingrowth:
Porosity Analysis
Many medical implants use porous structures to promote bone ingrowth. Proper analysis requires:
- Porosity percentage measurement (ASTM E562)
- Pore size distribution
- Pore shape and connectivity
- Pore uniformity assessment
Porous composite structure, 200X magnification. Proper preparation preserves pore structure for accurate analysis in medical implants.
Preparation Challenges
- Use vacuum impregnation for porous samples
- Consider castable mounting to fill pores
- Avoid pulling out material during grinding/polishing
- Use appropriate polishing media and techniques
- Document any preparation artifacts
Additively Manufactured Implants
Additive manufacturing (3D printing) is increasingly used for custom implants:
Build Structure Analysis
- Layer boundary assessment
- Build direction effects
- Melt pool structure
- Grain growth patterns
Defect Analysis
- Porosity assessment (lack of fusion, keyhole porosity)
- Crack detection
- Inclusion assessment
- Support structure remnants
Microstructure Evaluation
- Grain structure in different regions
- Phase distribution
- Heat treatment effects
- Comparison with specification requirements
Coating and Surface Modification
Many implants have coatings or surface modifications:
Coating Analysis
- Coating thickness measurement
- Coating uniformity
- Coating-substrate interface evaluation
- Coating porosity and defects
- Coating adhesion assessment
Surface Modification
- Modified layer thickness
- Modification depth uniformity
- Interface characteristics
- Microstructure changes in modified zone
Mechanical Property Correlation
Relate microstructure to mechanical properties:
- Hardness measurements (microhardness traverses)
- Correlation with tensile properties
- Fatigue performance indicators
- Wear resistance assessment
Biocompatibility-Related Features
Assess features that affect biocompatibility:
- Surface oxide layer (for titanium)
- Surface contamination
- Microstructure uniformity
- Absence of toxic phases
- Proper heat treatment (for alloys)
Regulatory Compliance Considerations
Medical device metallography must comply with strict regulatory requirements. Understanding and following these requirements is essential for device approval and ongoing compliance.
FDA Requirements (United States)
The U.S. Food and Drug Administration (FDA) regulates medical devices:
Quality System Regulation (21 CFR Part 820)
- Requires documented procedures for all processes
- Mandates equipment calibration and maintenance
- Requires personnel training and qualification
- Emphasizes traceability and documentation
- Requires validation of processes and methods
- Mandates corrective and preventive action (CAPA) systems
Design Controls (21 CFR 820.30)
- Metallographic analysis must be part of design validation
- Material specifications must be verified
- Process validation requires metallographic evidence
- Design changes require re-validation
ISO 13485 Requirements
ISO 13485 is the international quality management standard for medical devices:
- Requires documented quality management system
- Mandates risk management (ISO 14971)
- Requires validation of processes
- Emphasizes traceability
- Requires management of suppliers
- Mandates corrective and preventive actions
Documentation Requirements
Comprehensive documentation is essential for regulatory compliance:
Procedure Documentation
- Documented sample preparation procedures
- Standard operating procedures (SOPs) for all methods
- Equipment operation and maintenance procedures
- Calibration records and schedules
Analysis Documentation
- Detailed sample preparation records
- All measurements and observations documented
- High-quality micrographs with proper magnification and scale bars
- Traceability from sample to report
- Review and approval signatures
- Retention of records per regulatory requirements
Report Requirements
- Clear identification of sample and device
- Methods used (referencing standards)
- Results with appropriate precision and accuracy
- Conclusions and recommendations
- Reviewer and approver identification
- Date and version control
Material Specifications
Medical device materials must meet specific specifications:
ASTM Standards for Medical Materials
- ASTM F67: Unalloyed titanium for surgical implant applications
- ASTM F136: Wrought titanium-6aluminum-4vanadium ELI (extra low interstitial) alloy
- ASTM F138: Stainless steel bar and wire for surgical implants
- ASTM F75: Cobalt-28chromium-6molybdenum alloy castings
- ASTM F1537: Wrought cobalt-28chromium-6molybdenum alloy
Verification Requirements
- Verify material composition (per specification)
- Confirm microstructure meets requirements
- Validate mechanical properties
- Check for compliance with biocompatibility requirements
Biocompatibility Standards
Biocompatibility is assessed per ISO 10993:
- Material characterization (Part 18)
- Cytotoxicity testing
- Sensitization assessment
- Systemic toxicity evaluation
- Implantation studies
Metallography supports biocompatibility assessment by ensuring proper material structure and absence of toxic phases or contamination.
Risk Management (ISO 14971)
Risk management is integral to medical device development:
- Identify material-related hazards
- Assess risks associated with material failures
- Implement controls (including metallographic verification)
- Monitor effectiveness of controls
- Document risk management activities
Audit Readiness
Maintain audit readiness:
- Organized documentation system
- Easy retrieval of records
- Clear traceability
- Trained personnel
- Calibrated and maintained equipment
- Validated procedures
Change Control
Any changes to materials, processes, or procedures require:
- Documentation of the change
- Impact assessment
- Validation of the change
- Regulatory notification if required
- Updated documentation
Specialized Sample Preparation Techniques
Medical device samples often require specialized preparation techniques to preserve critical features and meet regulatory requirements.
Sectioning
Sectioning medical device samples requires careful technique:
- Use appropriate cutting methods to minimize damage
- For porous structures, use careful sectioning to avoid pullout
- For coated samples, ensure sectioning doesn't delaminate coatings
- Document sectioning location and orientation
- Maintain cleanliness to avoid contamination
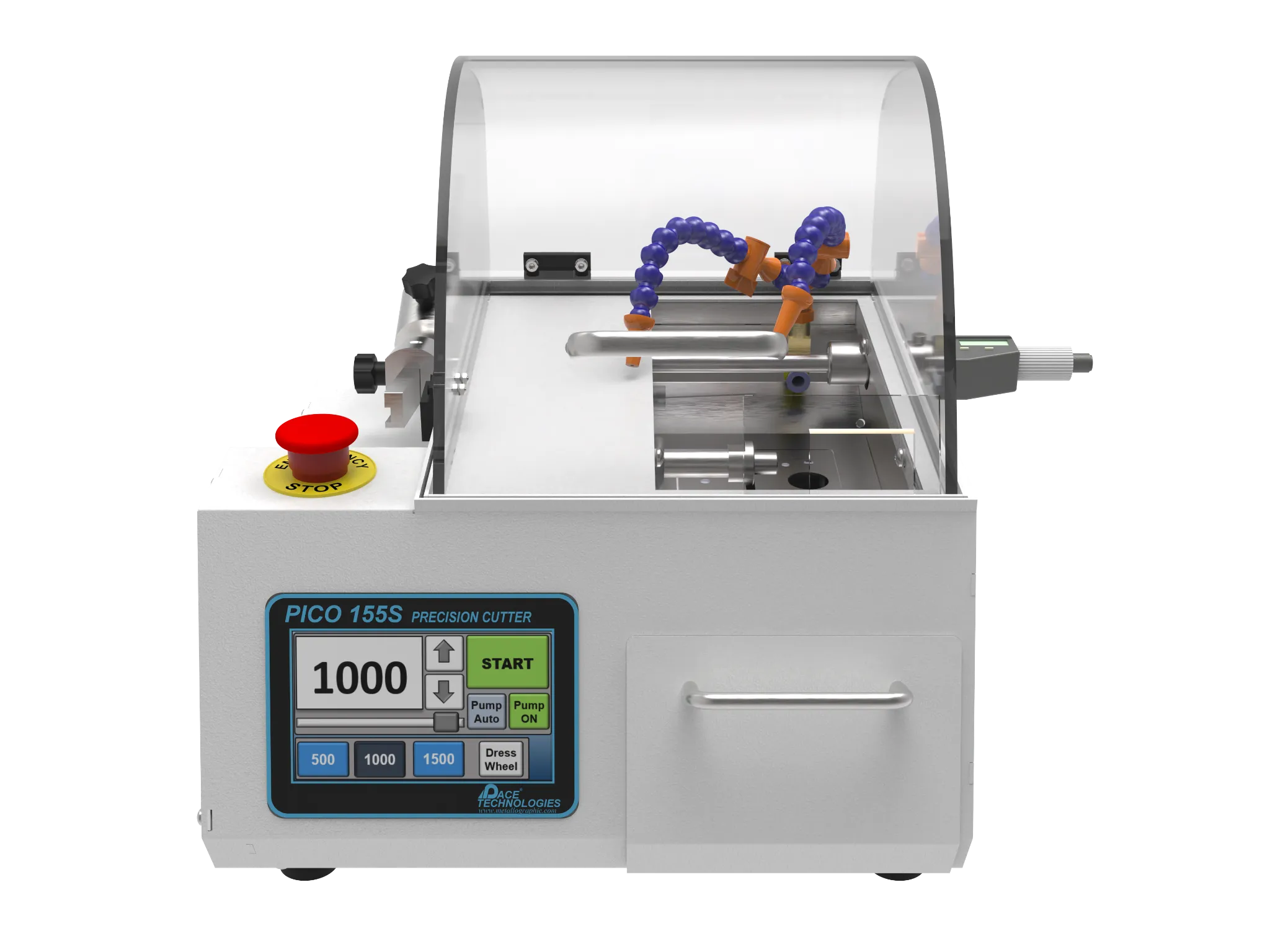
Example Products: Precision Wafering EquipmentLow-damage sectioning for medical device samples
For purchasing options and product specifications, see commercial supplier website.
Mounting
Mounting medical device samples requires special considerations:
- Use appropriate mounting methods based on sample type
- For porous samples, use vacuum impregnation or castable mounting
- For edge retention, consider nickel plating or specialized mounting
- Use mounting materials compatible with intended analysis
- Ensure mounting doesn't introduce contamination
Example Products: Castable Mounting SystemsVacuum and pressure mounting systems for porous medical device samples
For purchasing options and product specifications, see commercial supplier website.
Grinding and Polishing
Grinding and polishing require contamination control:
- Follow standard progressive procedures
- For titanium, use careful polishing to avoid smearing
- For hard materials (cobalt-chromium), use appropriate abrasives
- For porous structures, use gentle techniques to avoid pullout
- Maintain flat surfaces for accurate measurements
- Use clean, filtered polishing media
Example Products: Diamond Polishing Compoundssuitable diamond compounds for contamination-free polishing of medical device materials
For purchasing options and product specifications, see commercial supplier website.
Etching
Select etchants based on material and analysis requirements:
- Titanium: Kroll's reagent, Weck's reagent, anodizing
- Stainless steel (316L): Electrolytic oxalic acid, glyceregia
- Cobalt-chromium: Murakami's reagent, glyceregia
- Surface analysis: May require minimal or no etching
Safety: Many medical device etchants contain hazardous chemicals (HF, strong acids). Always use proper PPE and fume hoods.
Cleanliness and Contamination Control
- Use dedicated equipment when possible
- Thoroughly clean between samples
- Use filtered, clean polishing media
- Avoid cross-contamination
- Document cleaning procedures
- Consider disposable consumables for critical samples
Standards and References
ASTM Standards
- ASTM E3 - Standard Practice for Preparation of Metallographic Specimens
- ASTM E112 - Standard Test Methods for Determining Average Grain Size
- ASTM E384 - Standard Test Method for Microindentation Hardness of Materials
- ASTM E562 - Standard Test Method for Determining Volume Fraction by Systematic Manual Point Count
- ASTM F67 - Standard Specification for Unalloyed Titanium for Surgical Implant Applications
- ASTM F136 - Standard Specification for Wrought Titanium-6Aluminum-4Vanadium ELI Alloy
- ASTM F138 - Standard Specification for Wrought 18Chromium-14Nickel-2.5Molybdenum Stainless Steel Bar and Wire
- ASTM F75 - Standard Specification for Cobalt-28Chromium-6Molybdenum Alloy Castings
- ASTM F1537 - Standard Specification for Wrought Cobalt-28Chromium-6Molybdenum Alloy
ISO Standards
- ISO 13485 - Medical devices - Quality management systems
- ISO 14971 - Medical devices - Application of risk management
- ISO 10993 - Biological evaluation of medical devices
- ISO 5832 - Implants for surgery - Metallic materials
- ISO 643 - Steels - Micrographic determination of the apparent grain size
Regulatory References
- 21 CFR Part 820 - Quality System Regulation (FDA)
- 21 CFR Part 820.30 - Design Controls (FDA)
- EU MDR (European Medical Device Regulation)
- MDSAP (Medical Device Single Audit Program)
Additional Resources
- Medical device manufacturer specifications
- Industry best practices and technical papers
- Biocompatibility testing guidelines
- Regulatory guidance documents
Conclusion
Metallographic analysis for medical device applications requires specialized knowledge of biocompatible materials, surface finish characterization, implant material evaluation, and regulatory compliance. The unique requirements of medical devices, particularly implants, demand meticulous attention to contamination control, detailed documentation, and adherence to regulatory standards.
By following proper preparation techniques, maintaining comprehensive documentation, and staying current with regulatory requirements, metallographers contribute to the safety and effectiveness of medical devices that improve and save lives. The critical nature of medical device applications makes accuracy, thoroughness, and compliance essential in every aspect of the analysis.
Key Takeaways: Maintain strict contamination control, document everything thoroughly for regulatory compliance, understand biocompatibility requirements, use appropriate techniques for surface analysis, and stay current with regulatory standards. Patient safety depends on accurate and thorough metallographic analysis.